Behavioral Health Revenue Cycle Management
Build Steady Revenue Streams for Your Behavioral Health Practice
From complex patient needs to variable payer reimbursements, mastering the billing and credentialing processes is a must for your behavioral health practice. Discover how our dedicated team of account managers, including a single point of contact, can help your practice increase payments by closing the gaps in your revenue cycle and streamlining your credentialing and enrollment tasks.
Schedule a Consultation with a Behavioral Health RCM Expert
Are Your Current Behavioral Health RCM & Credentialing Solutions Limiting Your Cash Flow?
Unlike traditional medical billing, behavioral health RCM is not an easily navigable process — especially for an in-house billing team. Rather than simple coding and billing, many practices face reimbursement roadblocks from payers who are reluctant to provide equal attention to behavioral health services. Additionally, any errors or oversights in the credentialing process can seriously impact the ability to get paid. A free RCM audit will show you how Med USA’s behavioral health billing and credentialing solutions will optimize your collections and build steady revenue streams. Your audit will reveal:

Struggling to decrease A/R days, maximize billables and speed up payments?
Med USA specializes in partnering with psychiatry, psychology and other mental health practices to streamline billing processes and optimize cash flow – and we’ve been successfully doing it for more than 40 years. Learn how our team can help set your practice up for success by scheduling an RCM consultation.
Behavioral Health Practices that Partner with Med USA Typically Experience:
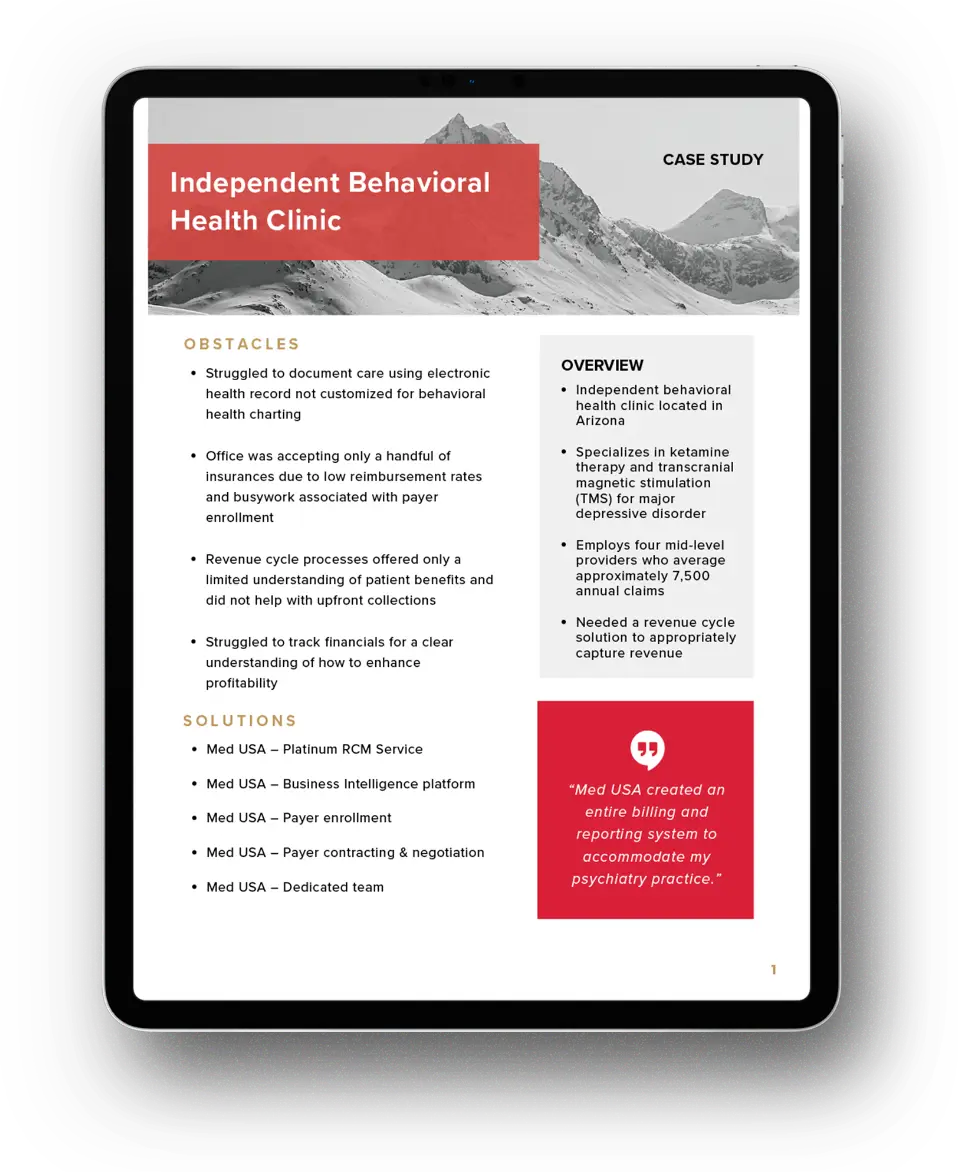
Client Success Stories
Discover how Med USA helped a behavioral health practice decrease A/R days, maximize billables, gain insight into key practice analytics and increase overall profitability.
“Med USA created an entire billing and reporting system to accommodate my psychiatry practice.”
Business Intelligence to Support Behavioral Health Practice Growth

Med USA’s cloud-based business intelligence platform positions behavioral health practices for growth by offering essential insights and tools to enhance operational efficiency and drive profitability, including:
Discover how your behavioral health practice can utilize data and other insights to quickly identify what’s working, what’s not, which processes to adjust and how to empower sustainable growth.
Trust Our Proven Solutions Certified By:


Reduce Claim Denials. Increase Reimbursements.
There are no long-term commitments for Med USA’s services and pricing is available on a simple per-application or per-task basis.
Testimonials
Professionals like you are talking about Med USA



