Provider Credentialing Services
How Much Is Your Current Credentialing & Enrollment Solution Holding Your Practice Back?

Credentialing and enrollment are complicated and time-intensive tasks. Errors in these essential processes can be fatal to a practice. That’s where Med USA comes in. As one of the nation’s top-rated credentialing companies, we provide every customer with a dedicated account manager who oversees every step of our provider enrollment and credentialing services, leaving no room for mistakes or missed deadlines. Schedule a one-payer sweep with a Med USA credentialing expert to uncover:

Trust Our Proven Solutions Certified By:


Data-Driven Credentialing Services for Providers
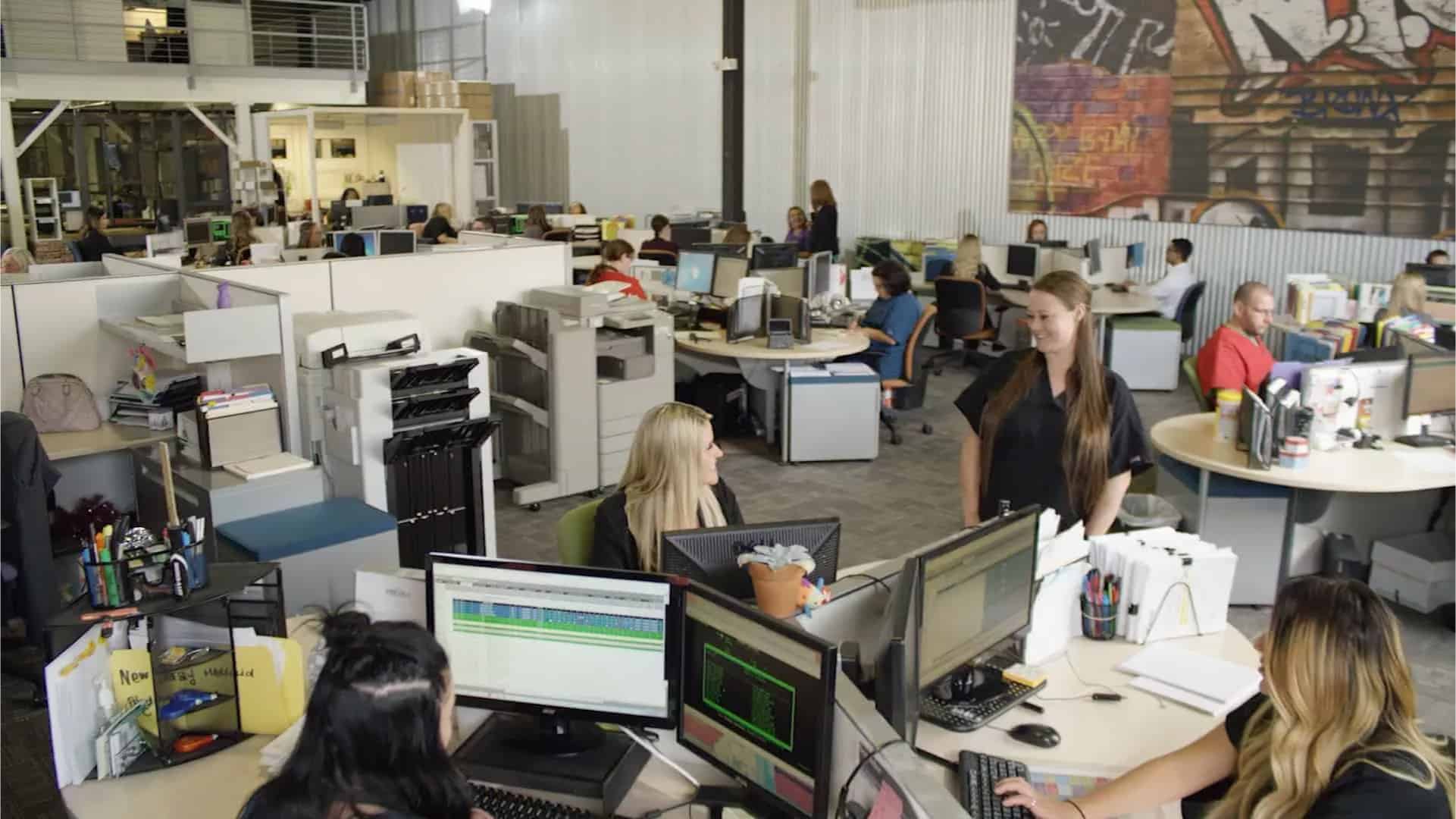
Med USA is one of the only provider credentialing companies that leverage real-time business intelligence to streamline RCM, A/R management, credentialing, enrollment, and every other process required to run a successful practice. Our highly customizable cloud-based practice analytics and business intelligence platform can help you gain visibility into credentialing workflows, increase administrative efficiency, minimize cash flow disruptions, and prevent future delays and bottlenecks.
Our Specialties
Provider Credentialing Services

Expirable Document Management Services
Re-Credentialing Services

Customized Credentialing Solutions
Med USA supports both newly graduated physicians and more experienced ones through our personalized and customized Provider Credentialing Solutions Services. We create customized solutions that allow us to consult, supplement, or provide fully managed credentialing services for your practice. Our team is highly trained and able to step in, analyze, and provide resourceful recommendations for your practices, then complete all the required applications and documentation. Our services are available to all medical professionals, including group practices, hospital-based physicians, non-physician practitioners, and laboratories.
Some of the customized solutions we offer include:
New Provider Credentialing Services
One of the most frustrating aspects of credentialing new providers is the number of requests they receive from staff who are inexperienced with how the credentialing process works. Med USA has developed an efficient on-boarding and collection process through our proprietary tool to facilitate the healthcare credentialing service for new providers as quickly and painlessly as possible. Our process encompasses the collection of provider data, supporting documentation and signatory needs which gives us everything to complete applications and submit in a timely manner.
Begin the Medical Credentialing Process Early


It is best to start any process as early as possible. Credentialing can be a long process and can take up to 90 days or longer depending on each payer’s timelines.
Lately, more payers have lengthened their timelines considerably and have been expanding their enrollment requirements to include Non-Physician Practitioners (NPP). Med USA Provider Credentialing consist of a time-tested proprietary process and a highly trained team ready to help support you through the navigation of the complicated maze of provider enrollment and credentialing. We can help you enroll a new hire, transition from one practice to another, or even set up enrollment to a new group. We will take care of the details so that you can take care of your patients.


The Details Matter
We worry about the details, so you don’t have to:
Stay Up To Date
Med usa helps you stay up to date and current on:
In-House Compliance Experts for a More Efficient, Scalable Medical Practice

With over 40 years in the industry as a provider and insurance credentialing company, we’ve helped countless healthcare providers across the country bill more efficiently and achieve financial transparency. Our dedicated team of medical billing experts is here to answer any questions you may have about physician credentialing services, whether you operate a lab, urgent care center, skilled nursing facility, hospital, or provider group!
-
CHARGE POSTING
-
PATIENT CONTACT
-
INSURANCE REIMBURSEMENT
-
REAL-TIME ANALYTICS
-
REIMBURSEMENT & PAYER MANAGEMENT

Get Ahead and Stay Up to Date on Your Credentialing Tasks
Credentialing can be a long process and can take up to 90 days or longer depending on each payer’s timelines — meaning it’s crucial to start as early as possible. Lately, more payers have lengthened their timelines considerably and have been expanding their enrollment requirements to include Non-Physician Practitioners (NPP).
Med USA Provider Credentialing consists of a time-tested proprietary process and a highly trained team ready to help you navigate the complex maze of provider enrollment and credentialing. We can help you enroll a new hire, transition from one practice to another, or even set up enrollment to a new group. We will take care of the details so that you can take care of your patients.
Discover the easier way to:
Eliminate Errors. Reduce Claim Denials.
Provider credentialing and enrollment are complex and time-consuming processes that can strain an already overworked billing team. Our provider credentialing experts are here to help you complete these tasks accurately and on time. With our dedicated team keeping track of all deadlines, requirements, and other potential reimbursement barriers, your practice can do more with less.
Optimize Your Practice Today
How much revenue is your practice missing?
Reach out to see how our team can help!
Testimonials
Professionals like you are talking about Med USA



