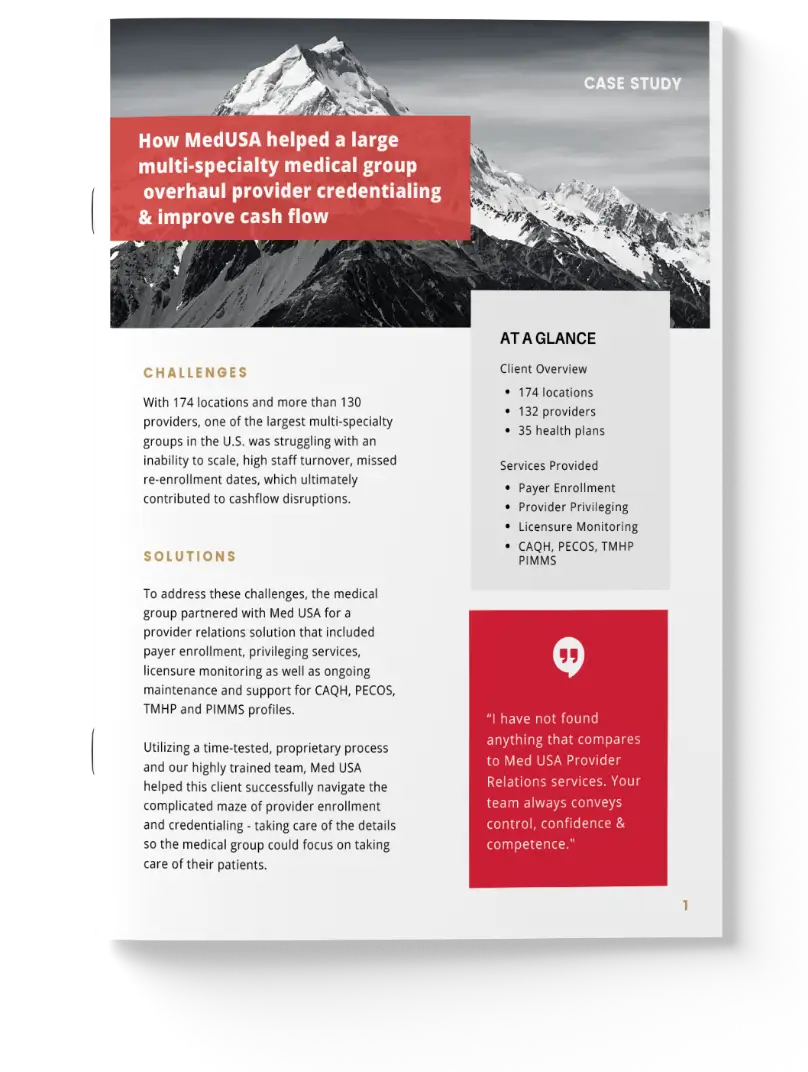
How a Multi-Specialty Medical Group Achieved a 78% Decrease in Days to Provider Enrollment
With over 130 providers to credential, enroll, and privilege, one of the largest multi-specialty groups in the U.S. struggled to scale PR operations, leading to major cash flow leaks. Learn how Med USA’s proprietary PR solutions accelerated enrollment and privileging to restore a healthy cash flow.
Download the Case Study
Revenue Cycle Management
-
CHARGE POSTING
-
PATIENT CONTACT
-
INSURANCE REIMBURSEMENT
-
REAL-TIME ANALYTICS
-
REIMBURSEMENT & PAYER MANAGEMENT
Provider Relations
-
Credentialing & Enrollment
-
Provider re-credentialing
-
Contracting payer enrollment
-
Provider privileging
-
Expirable document management
On the Blog
Stay current on best practices for revenue cycle management, credentialing, and healthcare compliance